| Korean J Health Promot > Volume 17(2); 2017 > Article |
|
ņÜöņĢĮ
Background:
This study investigated factors related to awareness of cardio-cerebrovascular disease (CCVD) in a large Korean general population.
Methods:
Data for 228,781 subjects older than 19 years in 253 cities, counties, and districts were collected from the 2013 Community Health Survey in Korea. Associations between socio-demographics, health behaviors, comorbidities, and awareness of CCVD were examined using the chi-squared test and multiple logistic regression analysis. A total of 219,461 subjects were included in the final analysis after excluding subjects with null responses to any questions.
Results:
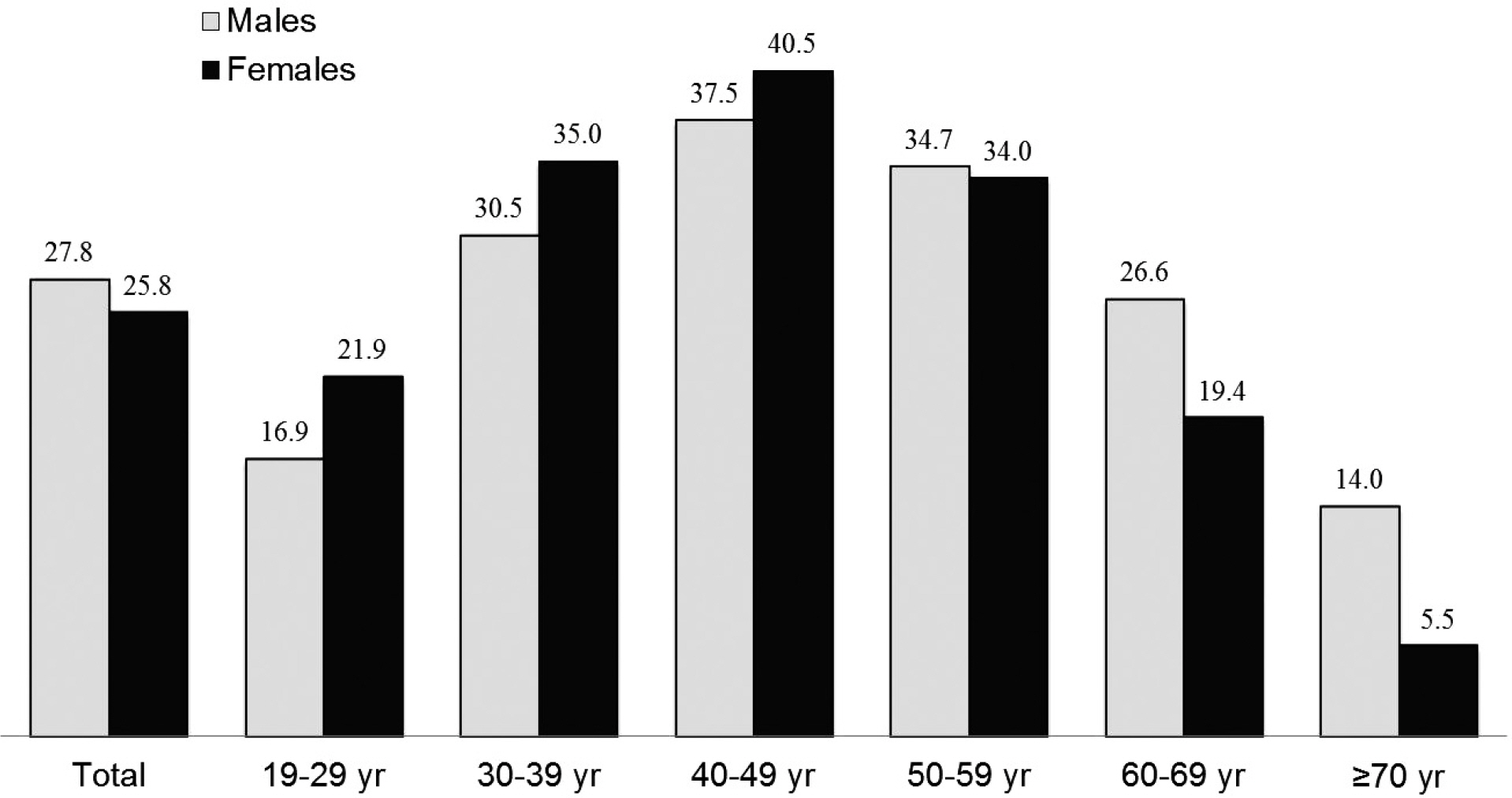
The awareness of CCVD was 26.7% in the total population (27.8% in males, 25.8% in females). Of the significant associating factors, the odds ratios for awareness of CCVD were two-fold higher in people aged 40-49 years, 50-59 years, and 60-69 years (ref. 19-29 years), living in Chungbuk provinces (ref. Seoul), higher education (ref. non-formal education), and diagnosed with angina pectoris (ref. non-diagnosed), as compared to their individual reference groups.
Figure┬Ā1.
The age-specific experience rate of exposure to public relations media on cardio-cerebrovascular disease according to gender.
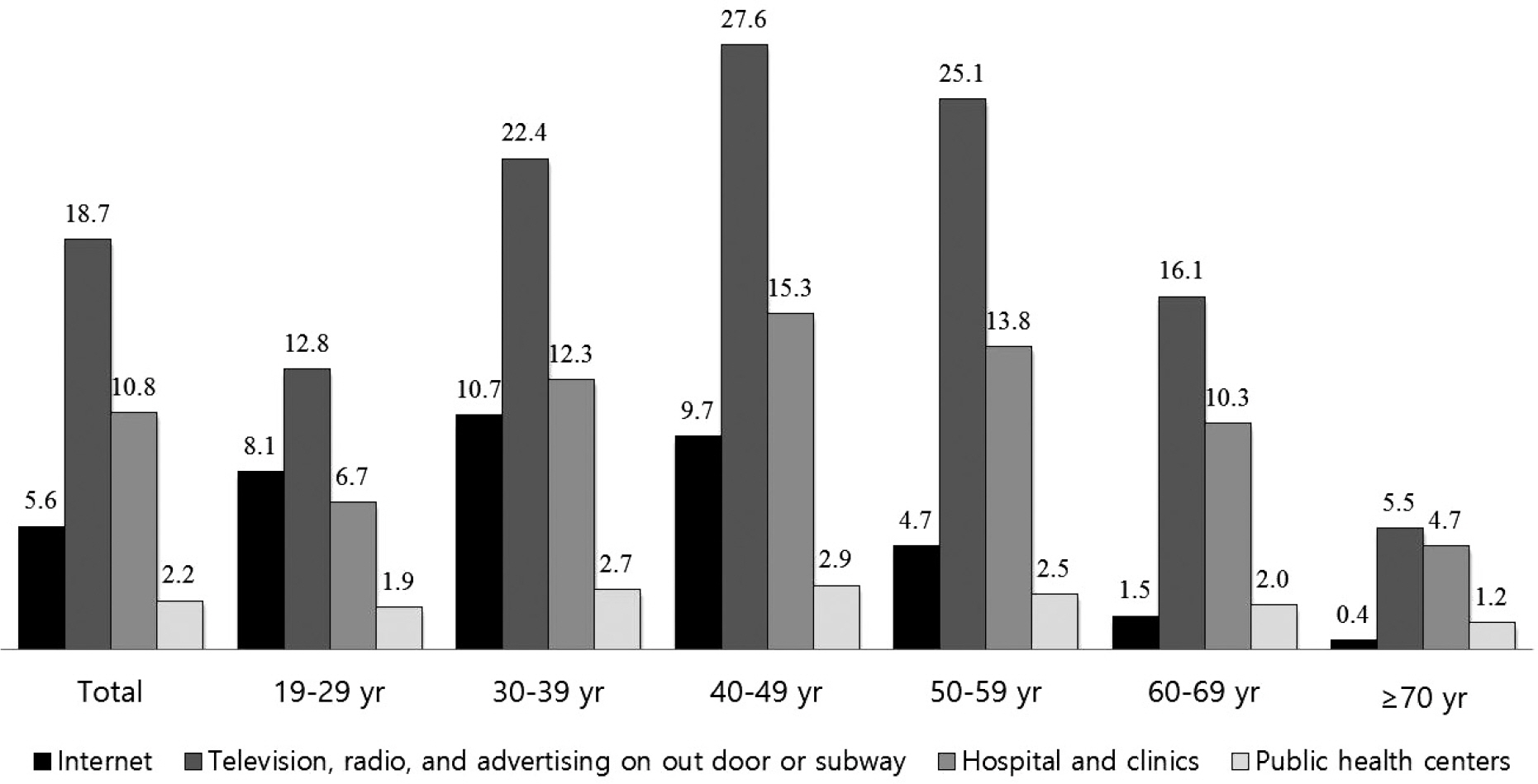
Figure┬Ā2.
The age-specific experience rate of exposure to public relations media on cardio-cerebrovascular disease according to pathway of experience.
Table┬Ā1.
Socio-demographic characteristics according to awareness of cardio-cerebrovascular disease
Table┬Ā2.
Health behaviors and comorbidities according to awareness of cardio-cerebrovascular disease
Table┬Ā3.
Associating factors for awareness of cardio-cerebrovascular disease using multivariate logistic regression analysis
Values are presented as odds ratio (95% confidence interval). Adjusted for gender, age, metropolitan cities and provinces, location of residence, occupation, education level, marital status, monthly household income, the National Basic Livelihood Security, smoking status, drinking frequency, body mass index, hypertension, diabetes, dyslipidemia, stroke, myocardial infarction, and angina pectoris.
Table┬Ā4.
Gender- and age-specific odds ratio (95% confidence interval) for awareness of cardio-cerebrovascular disease using multivariate logistic regression analysis
Adjusted for metropolitan cities and provinces, location of residence, occupation, education level, marital status, monthly household income, the National Basic Livelihood Security, smoking status, drinking frequency, body mass index, hypertension, diabetes, dyslipidemia, stroke, myocardial infarction, and angina pectoris.
REFERENCES
1.. Korea National Statistics Korea. Causes of Death in South Korea, 2014 [Internet]. Daejeon: Korea National Statistics Office website; 2015. [Accessed Aug 9, 2016]. Available from:. http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1012.
2.. Hannan EL, Zhong Y, Jacobs AK, Holmes DR, Walford G, Venditti FJ, et al. Effect of onset-to-door time and door-to-balloon time on mortality in patients undergoing percutaneous coronary interventions for st-segment elevation myocardial infarction. Am J Cardiol 2010;106(2):143-7.


3.. Gumbinger C, Reuter B, Stock C, Sauer T, Wieth├Člter H, Bruder I, et al. Time to treatment with recombinant tissue plasminogen activator and outcome of stroke in clinical practice: retrospective analysis of hospital quality assurance data with comparison with results from randomised clinical trials. BMJ 2014;348:g3429.



4.. McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol 2006;47(11):2180-6.


5.. Yeo LL, Paliwal P, Teoh HL, Seet RC, Chan BP, Liang S, et al. Timing of recanalization after intravenous thrombolysis and functional outcomes after acute ischemic stroke. JAMA Neurol 2013;70(3):353-8.


6.. Alberts MJ, Perry A, Dawson DV, Bertels C. Effects of public and professional education on reducing the delay in presentation and referral of stroke patients. Stroke 1992;23(3):352-6.


7.. Khan MS, Jafary FH, Faruqui AM, Rasool SI, Hatcher J, Chaturvedi N, et al. High prevalence of lack of knowledge of symptoms of acute myocardial infarction in Pakistan and its contribution to delayed presentation to the hospital. BMC Public Health 2007;7:284.




8.. Kim YS, Park SS, Bae HJ, Cho AH, Cho YJ, Han MK, et al. Stroke awareness decreases prehospital delay after acute ischemic stroke in Korea. BMC Neurol 2011;11:2.




9.. Pancioli AM, Broderick J, Kothari R, Brott T, Tuchfarber A, Miller R, et al. Public perception of stroke warning signs and knowledge of potential risk factors. JAMA 1998;279(16):1288-92.


10.. Samsa GP, Cohen SJ, Goldstein LB, Bonito AJ, Duncan PW, Enarson C, et al. Knowledge of risk among patients at increased risk for stroke. Stroke 1997;28(5):916-21.


11.. Naegeli B, Radovanovic D, Rickli H, Erne P, Seifert B, Duvoisin N, et al. Impact of a nationwide public campaign on delays and outcome in Swiss patients with acute coronary syndrome. Eur J Cardiovasc Prev Rehabil 2011;18(2):297-304.



12.. Bray JE, Stub D, Ngu P, Cartledge S, Straney L, Stewart M, et al. Mass media campaigns' influence on prehospital behavior for acute coronary syndromes: an evaluation of the Australian Heart Foundation's warning signs campaign. J Am Heart Assoc 2015;4(7):e001927.



13.. Lee YH, Park HY, Lee HS, Ha YS, Cheong JS, Cho KH, et al. Effects of community-based stroke education and advocacy on the time from stroke onset to hospital arrival in ischemic stroke patients. J Korean Neurol Assoc 2015;33(4):265-71.


14.. Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation 2006;114(2):168-82.


15.. Mikul├Łk R, Bunt L, Hrdlicka D, Dusek L, V├Īclav├Łk D, Kryza J. Calling 911 in response to stroke: a nationwide study assessing definitive individual behavior. Stroke 2008;39(6):1844-9.


16.. Fussman C, Rafferty AP, Lyon-Callo S, Morgenstern LB, Reeves MJ. Lack of association between stroke symptom knowledge and intent to call 911: a population-based survey. Stroke 2010;41(7):1501-7.


17.. Kang YW, Ko YS, Kim YJ, Sung KM, Kim HJ, Choi HY, et al. Korea community health survey data profiles. Osong Public Health Res Perspect 2015;6(3):211-7.



18.. Kim HS, Lee H, Kim K, Park HK, Park KS, Kang GW, et al. The general public's awareness of early symptoms of and emergency responses to acute myocardial infarction and related factors in South Korea: a national public telephone survey. J Epidemiol 2016;26(5):233-41.


19.. Oh GJ, Moon J, Lee YM, Park HK, Park KS, Yun WY, et al. public awareness of stroke and its predicting factors in Korea: a national public telephone survey, 2012 and 2014. J Korean Med Sci 2016;31(11):1703-10.




20.. Lee YH, Kim YT, Oh GJ, Kim NH, Cho KH, Park HY, et al. Effects of community-based education and advocacy intervention on public awareness about the warning signs of stroke and the golden window of time. Korean J Health Educ Promot 2015;32(1):1-10.

21.. Park MH, Jo SA, Jo I, Kim E, Eun SY, Han C, et al. No difference in stroke knowledge between Korean adherents to traditional and western medicine - the AGE study: an epidemiological study. BMC Public Health 2006;6:153.




22.. Kim EM, Hwang SY, Kim AL. Knowledge of stroke and heart attack symptoms and risk factors among rural elderly people: a questionnaire survey. Korean Circ J 2011;41(5):259-64.



23.. Kopec G, Sobien B, Podolec M, Dziedzic H, Zarzecka J, Loster B, et al. Knowledge of a patient-dependant phase of acute myocardial infarction in Polish adults: the role of physician's advice. Eur J Public Health 2011;21(5):603-8.


24.. Swanoski MT, Lutfiyya MN, Amaro ML, Akers MF, Huot KL. Knowledge of heart attack and stroke symptomology: a cross-sectional comparison of rural and non-rural US adults. BMC Public Health 2012;12:283.




25.. Bray JE, Johnson R, Trobbiani K, Mosley I, Lalor E, Cadilhac D. National Stroke Foundation. Australian public's awareness of stroke warning signs improves after national multimedia campaigns. Stroke 2013;44(12):3540-3.


26.. Goff DC Jr, Sellers DE, McGovern PG, Meischke H, Goldberg RJ, Bittner V, et al. Knowledge of heart attack symptoms in a population survey in the United States: The REACT trial. rapid early action for coronary treatment. Arch Intern Med 1998;158(21):2329-38.

27.. Quah JL, Yap S, Cheah SO, Ng YY, Goh ES, Doctor N, et al. Knowledge of signs and symptoms of heart attack and stroke among Singapore residents. Biomed Res Int 2014;2014:572425.




28.. Kim YS, Park SS, Bae HJ, Heo JH, Kwon SU, Lee BC, et al. Public awareness of stroke in Korea: a population-based national survey. Stroke 2012;43(4):1146-9.


29.. Nicol MB, Thrift AG. Knowledge of risk factors and warning signs of stroke. Vasc Health Risk Manag 2005;1(2):137-47.



30.. Fang J, Gillespie C, Keenan NL, Greenlund KJ. Awareness of heart attack symptoms among US adults in 2007, and changes in awareness from 2001 to 2007. Future cardiol 2011;7(3):311-20.


31.. Thun MJ, Carter BD, Feskanich D, Freedman ND, Prentice R, Lopez AD, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med 2013;368(4):351-64.



32.. O'Keefe JH, Bybee KA, Lavie CJ. Alcohol and cardiovascular health: the razor-sharp double-edged sword. J Am Coll Cardiol 2007;50(11):1009-14.

33.. Lee YH, Shin MH, Kweon SS, Choi JS, Park MS, Cho KH, et al. Awareness of stroke warning signs and risk factors: result of a 2010 community survey in Gwangju metropolitan city. J Korean Neurol Assoc 2012;30(1):26-32.
-
METRICS

-
- 7 Crossref
- 0 Scopus
- 1,090 View
- 3 Download
- Related articles

 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


