Association of Smoking Status and High Density Lipoprotein-Cholesterol in Males in the Fifth Korea National Health and Nutrition Examination Survey
-
In Kyung Jung

- Received July 21, 2017 Accepted September 11, 2017
- ABSTRACT
-
- Background
- The patients with metabolic syndrome had shown low high density lipoprotein-cholesterol (HDL-C) and smoking had been reported to be an independent risk factor for low HDL-C. This study aimed to study the association of smoking status and low HDL-C in general population of Korea.
- Methods
- Frequency analysis and descriptive statistics for general characteristics and chi-square test for the association of smoking status and low HDL-C were used. Then, logistic regression analyses for the effect of smoking on low HDL-C and general linear method for HDL-C estimates were used.
- Results
- Univariate regression showed that smoking status showed an association with low HDL-C. Prevalence of low HDL-C was 29.4±0.3% of Korean males in their twenties or over, and low HDL-C possibilities of current and past-smokers compared with non-smokers were odds ratio 1.345 and 1.123 respectively. After adjustments with sociodemographic factors, physical activity, body mass index (BMI), and age, the low HDL-C possibility of current-smokers was 1.328 times higher and for past-smokers was 0.892 times than non-smokers (P<0.05). The HDL-C concentration of current-smokers was 1.009 mg/dL lower than non-smokers', whereas that of past-smokers' was 0.478 mg/dL higher than non-smokers'. HDL-C concentration decreased 0.922 mg/dL for every 1 unit of BMI increase and 0.080 mg/dL for every 1-year age increase (P<0.05).
- Conclusions
- In this study using general population, HDL-C showed significant association with smoking status. The occupation, BMI and age also had significant associations. Conclusively, the possible strategies to maintain serum HDL-C include cessation of smoking, increase of physical exercise, and weight loss.
- REFERENCES
- REFERENCES
- 1. Ge P, Dong C, Ren X, Weiderpass E, Zhang C, Fan H, et al. The high prevalence of low HDL-cholesterol levels and dyslipidemia in rural populations in Northwestern China. PLoS One 2015;10(12):e0144104.
[Article] [PubMed] [PMC]2. Rosenson RS, Brewer HB, Rader DJ. Lipoproteins as biomarkers and therapeutic targets in the setting of acute coronary syndrome. Circ Res 2014;114(12):1880-1889.
[Article] [PubMed]3. Heinecke JW. The HDL proteome: a marker--and perhaps mediator--of coronary artery disease. J Lipid Res 2009;50:S167-S171.
[Article] [PubMed] [PMC]4. Redondo S, Martínez-González J, Urraca C, Tejerina T. Emerging therapeutic strategies to enhance HDL function. Lipids Health Dis 2011;10:175.
[Article] [PubMed] [PMC]5. Makariou S, Liberopoulos E, Florentin M, Lagos K, Gazi I, Challa A, et al. The relationship of vitamin D with non-traditional risk factors for cardiovascular disease in subjects with metabolic syndrome. Arch Med Sci 2012;8(3):437-443.
[Article] [PubMed] [PMC]6. Rosenson RS. Low HDL-C: a secondary target of dyslipidemia therapy. Am J Med 2005;118(10):1067-1077.
[Article] [PubMed]7. Auwerx J, Bouillon R, Kesteloot H. Relation between 25-hydroxyvitamin D3, apolipoprotein A-I, and high density lipoprotein cholesterol. Arterioscler Thromb 1992;12(6):671-674.
[Article] [PubMed]8. Vimaleswaran KS, Cavadino A, Hyppönen E. APOA5 genotype influences the association between 25-hydroxyvitamin D and high density lipoprotein cholesterol. Atherosclerosis 2013;228(1):188-192.
[Article] [PubMed]9. Schnatz PF, Nudy M, O'Sullivan DM, Jiang X, Cline JM, Kaplan JR, et al. Coronary artery vitamin D receptor expression and plasma concentrations of 25-hydroxyvitamin D: their association with atherosclerosis. Menopause 2012;19(9):967-973.
[PubMed] [PMC]10. Gordon DJ, Probstfield JL, Garrison RJ, Neaton JD, Castelli WP, Knoke JD, et al. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation 1989;79(1):8-15.
[Article] [PubMed]11. Escolà-Gil JC, Julve J, Griffin BA, Freeman D, Blanco-Vaca F. HDL and lifestyle interventions. Handb Exp Pharmacol 2015;224:569-592.
[PubMed]12. Tosheska Trajkovska K, Topuzovska S. High-density lipoprotein metabolism and reverse cholesterol transport: strategies for raising HDL cholesterol. Anatol J Cardiol 2017;18(2):149-154.
[PubMed] [PMC]13. Kontush A, Lindahl M, Lhomme M, Calabresi L, Chapman MJ, Davidson WS. Structure of HDL: particle subclasses and molecular components. Handb Exp Pharmacol 2015;224:3-51.
[Article] [PubMed]14. Freeman DJ, Caslake MJ, Griffin BA, Hinnie J, Tan CE, Watson TD, et al. The effect of smoking on post-heparin lipoprotein and hepatic lipase, cholesteryl ester transfer protein and lecithin: cholesterol acyl transferase activities in human plasma. Eur J Clin Invest 1998;28(7):584-591.
[Article] [PubMed]15. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2010: Korea National Health and Nutrition Examination Survey (KNHANES V-1) [Internet]. Cheongwon: Korea Centers for Disease Control and Prevention; 2011;Accessed Apr 10, 2017]. Available from: https://knhanes.cdc.go.kr/knhanes/sub03/sub03_02_02.do16. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2) [Internet]. Cheongwon: Korea Centers for Disease Control and Prevention; 2012;Accessed Apr 10, 2017]. Available from: https://knhanes.cdc.go.kr/knhanes/sub03/sub03_02_02.do17. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2012: Korea National Health and Nutrition Examination Survey (KNHANES V-3) [Internet]. Cheongwon: Korea Centers for Disease Control and Prevention; 2013;Accessed Apr 10, 2017]. Available from: https://knhanes.cdc.go.kr/knhanes/sub03/sub03_02_02.do18. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 2014;43:69-77.
[Article] [PubMed] [PMC]19. Ni WQ, Liu XL, Zhuo ZP, Yuan XL, Song JP, Chi HS, et al. Serum lipids and associated factors of dyslipidemia in the adult population in Shenzhen. Lipids Health Dis 2015;14:71.
[Article] [PubMed] [PMC]20. Cugnetto ML, Saab PG, Llabre MM, Goldberg R, McCalla JR, Schneiderman N. Lifestyle factors, body mass index, and lipid profile in adolescents. J Pediatr Psychol 2008;33(7):761-771.
[Article] [PubMed] [PMC]21. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009;120(16):1640-1645.
[Article] [PubMed]22. Yun YM, Song J, Ji M, Kim JH, Kim Y, Park T, et al. Calibration of high-density lipoprotein cholesterol values from the Korea National Health and Nutrition Examination survey data, 2008 to 2015. Ann Lab Med 2017;37(1):1-8.
[Article] [PubMed] [PMC]23. Forey BA, Fry JS, Lee PN, Thornton AJ, Coombs KJ. The effect of quitting smoking on HDL-cholesterol - a review based on within-subject changes. Biomark Res 2013;1(1):26.
[Article] [PubMed] [PMC]24. Muratsubaki T, Hattori T, Li J, Fukudo S, Munakata M. Relationship between job stress and hypo-high-density lipoproteinemia of Chinese workers in Shanghai: the Rosai Karoshi Study. Chin Med J (Engl) 2016;129(20):2409-2415.
[PubMed] [PMC]25. Wang H, Peng DQ. New insights into the mechanism of low high-density lipoprotein cholesterol in obesity. Lipids Health Dis 2011;10:176.
[Article] [PubMed] [PMC]26. Zhao X, Zhang HW, Zhang Y, Li S, Xu RX, Sun J, et al. Impact of smoking status on lipoprotein subfractions: data from an untreated Chinese cohort. Biomed Environ Sci 2017;30(4):235-243.
[PubMed]
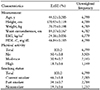
Table 4

Abbreviations: OR, odds ratio; HDL-C, lipoprotein-cholesterol; KNHANES V, the Fifth Korea National Health and Nutrition Examination Survey; CI, confidence interval; NA, not applicable; BMI, body mass index.
Values are presented as OR (95% CI).
aBelow 40 mg/dL.
bAdjusted by sociodemographic factors, e.g., region, housing, household income, education, and occupation.
cAdjusted by physical activity, BMI, and age.
dAdjusted by factors in Model 1 and Model 2.
eCalculated by complex sample logistic regression analysis.
Table 5

Abbreviations: HDL-C, high density lipoprotein cholesterol; KNHANES V, the Fifth Korea National Health and Nutrition Examination Survey; B, estimated mean; SE, standard error; CI, confidence interval; BMI, body mass index.
aModel: HDL-C (mg/dL)=intercept+smoking status+region+housing+household income+education+occupation+physical activity+BMI+age.
bThis parameter is set to zero because it is redundant.