| Korean J Health Promot > Volume 25(4); 2025 > Article |
|
ABSTRACT
Background
Methods
Results
Conclusions
AUTHOR CONTRIBUTIONS
Jun Woo KWON had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Author reviewed this manuscript and agreed to individual contributions.
Conceptualization, data curation, formal analysis, investigation, methodology, validation, writing–original draft, reviewing & editing: JWK.
Figure 1.
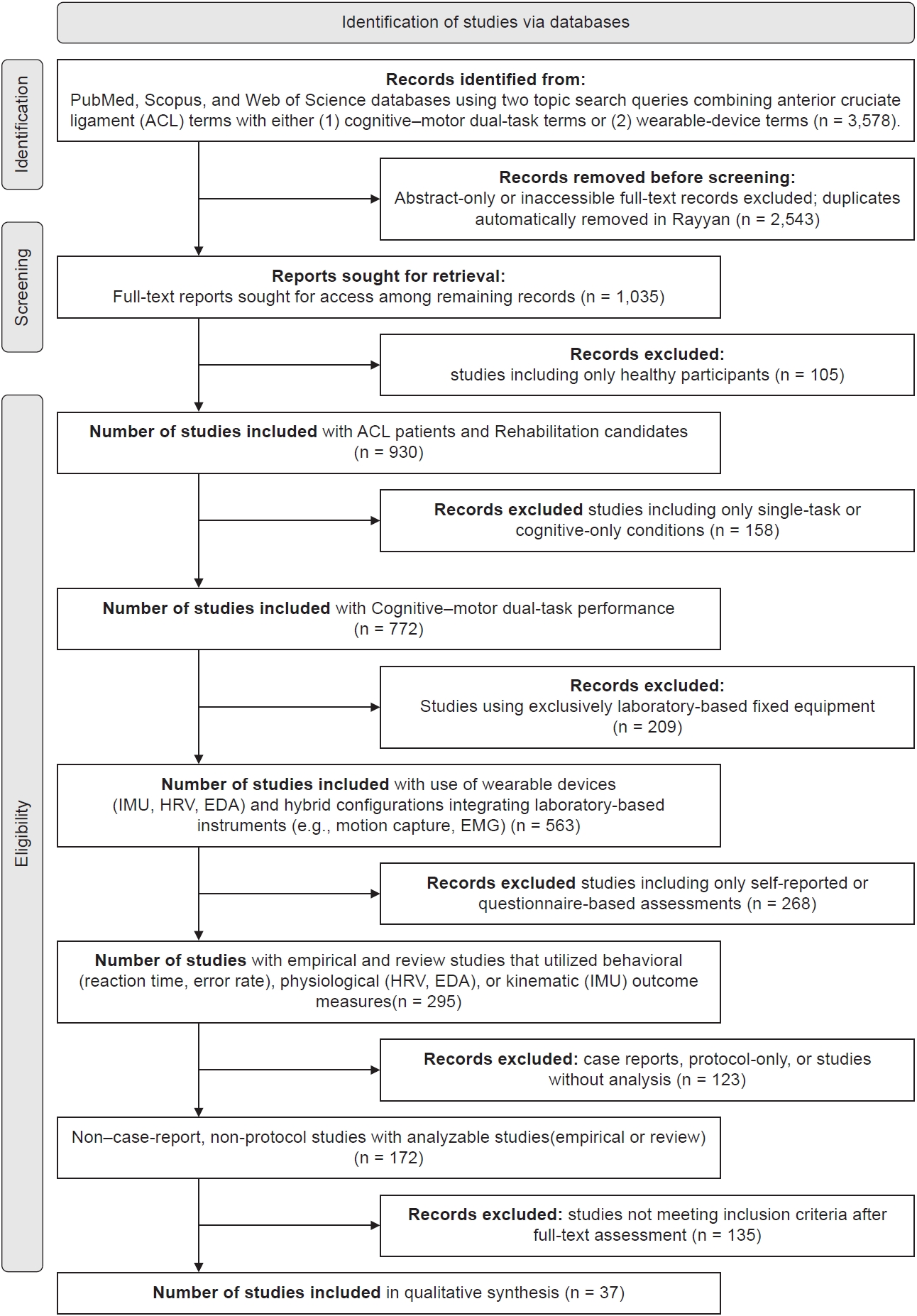
Table 1.
Table 2.
| Study (year) | Sample/injury (n) | Cognitive task (type, brief) | Motor task (type) | Device/modality (make/model if reported) | Key outcomes (behavioral/physiological/kinematic—brief) | Psychometric notes (ICC, SRM)/feasibility (setup time, field) |
|---|---|---|---|---|---|---|
| Marques et al. (2022) [12] | 11 studies (ACLR review) | – | Functional tasks (jump, gait, stairs) | IMUs (APDM, Xsens, Loadsol) | Bilateral asymmetry detected; wearables ≈ lab accuracy | ICC 0.80–0.96; field-portable |
| Morris et al. (2023) [13] | 191 college athletes (45% injured) | Serial subtraction, fluency | Reactive balance (Push & Release) | IMUs (Opal v2, APDM Inc.) | Dual-task TTS predicted injury risk (HR=1.36/250 msec) | Reliability and test duration not reported |
| Li et al. (2024) [14] | 60 (30 ACLR+30 controls) | – | Walk+hop tests | Flexible insole+IMU | ICC=0.91–0.98 vs. Vicon; LSI ≈ 88% | Portable system; battery life ≈ 12 hours |
| Nazary-Moghadam et al. (2019) [15] | 22 ACLD males+22 healthy controls | Auditory Stroop test (RT+error rate) | Treadmill walking at 3 speeds (low, self-selected, high) | Vicon motion capture (5 cameras, 100 Hz); knee kinematics (LyE) | ↑Gait speed → ↓knee flexion–extension LyE (ES=0.57); dual-task ↑RT in ACLD; cognitive load effect ns (P=0.07); ACLD prioritized gait over cognitive task | Within-session reliability reported in earlier companion study; single-session treadmill test; feasible lab setup |
| Jiménez-Martínez et al. [16] (2025) (systematic review) | 25 studies (≈ 670 healthy athletes, ACL risk context) | Dual-task/uncertainty manipulations (math subtraction, Stroop, reaction delay, visual distraction) | Jump-landing/sidestep/cutting | Motion capture+force plate (majority studies) | ↑Knee valgus angle and vGRF under high cognitive load → elevated ACL injury risk; slower RTs reported | Review synthesis (no ICC reported); lab-based tasks; field translation recommended |
| Jiménez-Martínez et al. [17] (2025) (cross-sectional study) | 30 ACLR+30 controls | Go/No-Go (proactive inhibitory control) | – | Computer task (SuperLab) | ↑RT, ↑commission errors, ↓accuracy in ACLR group (P<0.05) | Cross-sectional lab study; no ICC reported |
| Walker (2018) [18] | 10 ACLR | Exergame (implicit) | Narrow-based gait | Physilog IMU+EEG/EMG | ↓Stride time variability (η2=0.53) | Feasible |
| Majelan and Habibi (2022) [19] | 24 youth volleyball | Visual 5-digit reading | Tuck jump | Kinovea video | ↓Jump perf (η2=0.588) | Feasible |
| Avedesian (2024) [20] | Review of athlete studies (across levels) | Visual-motor RT, attention, WM | Jump-landing, cutting, gait | Smartboard, VR/AR, strobe eyewear, motion capture | ↓Knee flexion · ↑knee load with low cognition; slower RT ↑injury risk | Good test–retest; field-ready tools; VR setups less practical |
| Kacprzak et al. (2024) [21] | ACLR/review focus on neurosensory–motor integration | – | – | Narrative/theoretical | Hidden sensorimotor and cortical deficits after ACL injury; integration of sensory and motor networks emphasized | Conceptual; not quantitative |
| Akbari et al. (2023) [22] | 24 college soccer players (18 female, 6 male; 20±1 yr) | Heading a stationary soccer ball during jump (dual-task) | Drop vertical jump (30 cm box → jump & land) | 3D motion tracking+force plate | ↓Knee/hip/trunk flexion, ↓COM; ↑tibial shear, ↑trunk lat. flexion, ↑stiffness → ↑ACL risk | Reliable (r=0.63–0.91); lab-feasible but setup complex |
| Lin et al. (2025) [23] | 30 male division I athletes (CAI confirmed) | LED light reaction dual-task | Single-leg drop jump (30 cm) | Vicon (200 Hz), Kistler (1,000 Hz), Noraxon EMG (2,000 Hz) | ↑vGRF, ↑ankle inversion & rotation, ↑ROM; ↓rectus femoris EMG → ↓stability, ↑sprain risk | All completed; good repeatability; lab-feasible but complex setup |
| Yang et al. (2025) [24] | 22 males (11 healthy, 11 with ACL or meniscus injury) | None (pure EMG-based computational task; no behavioral dual-task) | Lower-limb motions: sitting, standing, and stair tasks (SIT, STA, STAND) | Surface EMG (4 muscles: BF, RF, VM, SEM), 1,000 Hz sampling | Dual-branch DL model (DBWCT-EMGNet): 99.86% accuracy, R2=0.98, RMSE=1.4°; TL improved patient performance from 85.5%→99.5% accuracy | <50 msec inference time; real-time feasible for rehab/exoskeleton applications |
| Song et al. (2023) [25] | Editorial | – | Various rehab | EMG, IMU, VR | Summary of 31 studies | – |
| Ness et al. (2020) [26] | 20 studies (review) | Stroop, n-back | Balance, gait | Force plate, IMU | ↑DTC | – |
| Disegni et al. (2025) [27] | Pro soccer ACLR | Visual recognition+ACL-RSI | Hop, RSA, match sim | Isokinetic, GPS | “11 to Perf” score | Field-feasible |
| Ghai et al. (2018) [28] | Healthy participants; Exp I: 15, Exp II: 20, Controls: 15 (age ≈ 23–27 yr) | Real-time auditory feedback (pitch–angle, amp–velocity) | Knee repositioning (40°, 75°) | XSENS IMU, headphones | ↓Error with sound; transient adaptation | 45 minutes; non-invasive; high compliance |
| Johnson et al. (2021) [29] | 20 healthy | – | SLS (perturbed) | Vicon+EMG | Flexed trunk ↑co-contraction | ICC>0.8 |
| Davidoviča et al. (2025) [30] | 32 youth football players (16 male/16 female; age 14.6±0.5 yr) | – | SLS+3 variations (front/middle/back; 60° knee flexion) | DAid smart socks, NOTCH IMUs, PLUX EMG | Strong correlations: hip adduction ↔ medial COP; knee flexion ↔ GM/GMx (ρ ≈ 0.84); COP2W ↔ GMx (ρ=−0.592); multiple moderate correlations between joint angles, COP and EMG | In-field feasible; non-invasive; session ≈ 45 minutes; high compliance |
| Lu et al. (2025) [31] | 16 healthy older adults (68.4±4.4 yr) | Serial subtraction (counting down by threes from random number 90–100; verbal dual task) | Obstacle crossing on 10 m walkway; obstacle height=10%, 20%, 30% of leg length | 8 camera motion system; 3 force plates | ↓Crossing speed (P=0.003); ↑leading & trailing toe-obstacle clearance (P<0.001); ↑pelvic anterior/posterior tilt, ↑swing hip abduction & knee flexion; ↓stance hip/knee adduction during dual-task | Normality (Shapiro–Wilk), homogeneity (Levene); two-way repeated ANOVA (task×height, α=0.05); power analysis lab setup feasible for older adults |
| Ptaszyk et al. (2025) [32] (scoping review) | ACL injury/ACLR | – | Pivot-shift, Lachman, hop/jump, gait, JPS | IMUs, accelerometers, force insoles, EM/inductive sensors | Accurate knee angle, load, and symmetry metrics | Easy to implement on-site, but standardization is needed |
| Lu et al. (2025) [33] | ACLR (n=20)+healthy (n=20) | – | Level walking gait at 3, 6, 12, 24 months post-op | 3D motion capture (Vicon MX, UK)+dual force plates (AMTI, USA) | Gradual gait symmetry recovery over 24 months; all angles & GRF normalized except persistent knee extension moment (pKEM) asymmetry | High validity; repeated-measures design; lab-based; feasible for longitudinal tracking |
| Kuroda et al. (2021) [34] | Narrative review | – | Various rehab | Robotics, IMU, VR | Improved ROM, motivation, adherence | No ICC or SRM; qualitative feasibility only |
| Baldazzi et al. (2022) [35] | 17 healthy male soccer players (21.5±3.2 yr) | – | SLS, CHT; 3 reps per limb (randomized order) | MIMU Gyko & foot; AMTI force plate | Angular velocity>acceleration metrics; dominant>nondominant limb; LSI within 85%–115% | Two-way mixed ICC (absolute agreement); MDC=SEM×1.96×√2; standardized 5-minute warm-up; 3 trials per task; field-feasible protocol |
| Aditya et al. (2025) [36] | 23 studies (MCI/dementia) | Subtraction, recall | Gait | IMU, fNIRS, MRI | ↓Speed, ↑variability, ↑PFC HbO2 | ICC=0.8–0.97 |
| Kiminski et al. (2025) [37] | 31 female athletes | Catch/fake throw | Drop landing+drill | Force plates+IMU | ↓vGRF 25%, ↑K:A ratio | ICC=0.90–0.91 |
| Kimura et al. (2017) [38] | 45 healthy adults | Visuospatial WM training | Elbow+knee torque tasks | EMG (Delsys)+torque chair | ↓FE2 errors (P<0.01), ↑WM capacity | 15 minutes×2 weeks feasible |
| Calisti et al. (2025) [39] | 43 (21 ACL-injured, 22 healthy; 19–36 yr) | – | Six jump-landings (single/bilateral) under fatigued & non-fatigued states | 10-camera Vicon, 2 force plates, OpenSim 4.3 | Fatigue ↓jump height (P=0.001) ↑Borg CR10; dataset supports analysis of joint kinematics & ACL deficits | Normality (Shapiro–Wilk), ANOVA; 2,199 valid trials; standardized lab setup |
| Detherage et al. (2021) [40] | 1 injured vs. 7 controls | Vision RT task | Training drills | Zephyr sensor+GPS | ↑BMI, slower RT, ↓HR recovery; ANS dysregulation | Feasible; single case |
| Forelli et al. (2025) [41] | Narrative review (ACLR population; no N reported) | Dual-task, neurocognitive drills | Quadriceps activation, gait, hop, strength | EMG, TMS, H-reflex, dynamometer, motion capture | Persistent AMI (↓cortical excitability, ↓CAR, asymmetry<90%), improved with NMES, BFR, dual-task rehab | No ICC reported; clinically feasible phase-based rehab; supports neurocognitive RTS framework |
| Krishnakumar et al. (2024) [42] | 71 studies (4 ACL groups) | – | Multi-tasks (walk, run, jump) | IMUs (Xsens, APDM, etc.) | ML-based models RMSE 0.02–0.04 BW; reliable across sagittal tasks | ICC variably reported; no pooled data; setup ~15–30 minutes typical |
| Calabrò et al. (2025) [43] | Narrative review (ACLR athletes/patients) | Dual-task (counting, reaction, decision) | Gait, balance, proprioceptive, neuromuscular training | Robotics, VR, biofeedback, wearable sensors, neuromodulation (TMS/TENS) | Neuroplasticity-based rehab ↓reinjury risk (9%–29%), ↑coordination & confidence | No ICC; qualitative; feasible but expert setup & cost limit |
| Ricupito et al. (2025) [44] | 17 ACLR | Reverse number recall | Triple hop distance | iPad+iPhones | ↓THD, DTC (full sample): healthy 6.49%–6.66%, post-op 4.32%–4.80%; | Time: NR; low-cost, single-session feasible |
| Rikken et al. (2024) [45] | 15 male basketball players (22.1±2.3 yr) | Visual-attention dual task - FitLights | 90° near-full-speed sidestep cut (energy-absorption phase: IC → peak knee flexion) | Xsens MVN IMU system (on-court); FitLights stimulus | ↓Hip flexion (IC & peak), ↓peak knee flexion, ↑peak hip external rotation; no ankle changes | No ICC/SRM reported; a-priori G*Power; SPM used; on-court IMU=higher ecological validity |
| Schwartz et al. (2025) [46] | 26 healthy adults | Visual-cognitive (go, inhibit, recall) | 5-10-5 & T-test | Dashr timing gates+FitLight | ICC: 0.75–0.99; DTE: −13%; no bias | Laboratory-based setup; no test-duration reported |
| Sherman et al. (2023) [47] | 20 ACLR vs. 20 controls | Go/No-Go visuomotor (virtual soccer) | Foot response | EEG (64ch LRP)+TMS | ↓LRP area, ↑error, ↑AMT, ↑effort | Lab-based EEG/TMS setup; no duration or cost reported |
| Strong and Markström (2025) [48] | 40 ACLR (8–59 months after ACL injury, the gender ratio is 1:1) | Cognitive-motor (decision, inhibition, WM) | Drop vertical jump | 8-cam Vicon+FP | ↓flexion, ↑vGRF, ↓injured load | Lab-based biomechanical assessment; no explicit ICC or duration reported in text |
This table summarizes study design elements, sensor modalities, and outcome domains across ACL injury, ACLR, or risk contexts. Each entry details cognitive and motor task types, wearable or laboratory measurement systems, and reported psychometric and feasibility information.
ACL, anterior cruciate ligament; ACLD, anterior cruciate ligament deficient; ACLR, anterior cruciate ligament reconstruction; AMI, arthrogenic muscle inhibition; AMT, active motor threshold; ANS, autonomic nervous system; AR, augmented reality; BF, biceps femoris; BFR, blood flow restriction; BMI, body mass index; BW, body weight; CAI, chronic ankle instability; CAR, central activation ratio; CHT, crossover hop test; COM, center of mass; COP, center of pressure; COP2W, two-dimensional center of pressure width; DL, deep learning; DTC, dual-task cost; DTE, dual-task effect; EEG, electroencephalography; EM, electromagnetic; EMG, electromyography; ES, effect size; Exp, experimental group; fNIRS, functional near-infrared spectroscopy; FP, force plate; GM, gluteus maximus; GMx, gluteus maximus; GPS, global positioning system; GRF, ground reaction force; HbO2, oxyhemoglobin; HR, hazard ratio; IC, initial contact; ICC, intraclass correlation coefficient; IMU, inertial measurement unit; JPS, joint position sense; K:A, knee-to-ankle ratio; lat., lateral; LED, light emitting diode; LRP, lateralized readiness potential; LSI, limb-symmetry index; LyE, Lyapunov exponent; MCI, mild cognitive impairment; MDC, minimal detectable change; MIMU, magnetic-inertial measurement unit; ML, machine learning; MRI, magnetic resonance imaging; NMES, neuromuscular electrical stimulation; NR, not reported; ns, not significant; PFC, prefrontal cortex; pKEM, peak knee extension moment; post-op, postoperative; rehab, rehabilitation; RF, rectus femoris; RMSE, root mean square error; ROM, range of motion; RSA, repeated sprint ability; RSI, return to sport after injury scale; RT, reaction time; RTS, return-to-sport; SEM, standard error of measurement; SIT, sit task; SLS, single-leg squat; SPM, statistical parametric mapping; SRM, standardized response mean; STA, stair task; STAND, stand task; TENS, transcutaneous electrical nerve stimulation; THD, triple hop for distance; TL, transfer learning; TMS, transcranial magnetic stimulation; TTS, time-to-stability; vGRF, vertical ground reaction force; VM, vastus medialis; VR, virtual reality; WM, working memory; η2, eta-squared effect size.
Table 3.
Synthesizes validity, reliability, responsiveness, and feasibility metrics of wearable and cognitive–motor tools extracted from Table 2. Each domain aggregates studies using similar measurement paradigms (e.g., IMU-based, force-plate, dual-task, neurocognitive, ML-driven systems).
ACL, anterior cruciate ligament; AMI, arthrogenic muscle inhibition; BW, body weight; corr, correlation coefficient; DTE, dual-task effect; EMG, electromyography; GPS, global positioning system; ICC, intraclass correlation coefficient; IMU, inertial measurement unit; MDC, minimal detectable change; ML, machine learning; N/A, not available; rehab, rehabilitation; RMSE, root mean square error; SRM, standardized response mean; vGRF, vertical ground reaction force; VR, virtual reality.
Table 4.
REFERENCES
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 188 View
- 10 Download
- ORCID iDs
-
Jun Woo KWON

https://orcid.org/0009-0006-0635-9649 - Related articles

 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


