Nurses’ Experiences with the Use of Electronic Nursing Record: A Qualitative Study
Article information
Abstract
Background
The electronic nursing record has contributed to improving nursing practice and ensuring nursing quality, but it is still incomplete in supporting nursing workflow. The purpose of this study is to explore the experience of using the electronic nursing record by nurses working in frontline care for trauma, emergency, and infectious disease-exposed patients.
Methods
The study employed a qualitative descriptive design and qualitative content analysis. In-depth interviews were conducted with 10 nurses working in emergency, trauma, and critical care units in the tertiary hospital.
Results
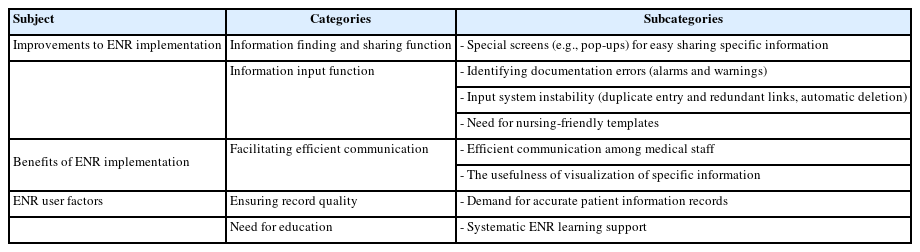
The nurses’ experiences with the use of the electronic nursing record emerged into three subjects (improvements to electronic nursing record implementation, benefits of electronic nursing record implementation, electronic nursing record user factors), five categories (information finding and sharing function, information input function, facilitating efficient communication, ensuring record quality, need for education), and eight subcategories.
Conclusions
Electronic nursing record supports the visualization of special information such as emergency and infection, and has the advantage of facilitating communication between medical staff. Both support better clinical decision-making. However, system instability and low nursing friendliness delay nursing work in the process of inputting, confirming, and sharing information. Copy-and-paste practices, poor quality of records, and insufficient electronic nursing record education were identified as factors to be changed on the user side. Improvement of nursing-friendly interfaces, optimization of nursing workflows, and participation of nurses in the improvement process are necessary. We should also focus on developing electronic nursing record education programs.
INTRODUCTION
Nurses have a critical responsibility for accurately documenting and communicating patient care information in clinical settings. Nurses, especially those caring for patients with high acuity, such as emergency rooms and intensive care units, have seen their workloads increase in the post-pandemic world [1-3].
Enhanced infection control, patient safety, and information security measures have complicated administrative procedures in nursing. Consequently, nurses have faced difficulties in managing nursing information [3]. In the role of recording and communicating patient information, the electronic nursing record (ENR) saves recording time, allowing nurses to dedicate more time to patient care. It also enhances the clarity, quantity, quality, availability, and continuity of information. The ENR has been emphasized as a crucial tool in delivering patient medical information due to its advantages in improving continuity of care [4]. In this regard, it is important to continuously monitor the effectiveness of the ENR in nursing tasks.
Electronic medical record (EMR) implementation technology has been developed worldwide, and research on EMR usability has been conducted steadily [5]. As EMR technology develops, it is important to use an EMR that supports nurses to reduce their burden in performing their work. A recent study targeting clinicians and nurses reported that although EMR brings efficiency to work, it also causes fatigue, errors, and burnout [6]. In addition, nurses are reported to feel psychological stress and time pressure due to lack of reliability and user friendliness of EMR [7]. Therefore, continuous improvement efforts are needed to save medical staff’s time and optimize treatment and nursing workflows [8].
Recent studies on EMR use involving nurses have been conducted on various dimensions, including the overall experience of using EMR [9], the copy & paste (C&P) function as part of the specific ENR function [10], the impact of EMR on nurse-patient interaction and communication quality [11], and the impact of ENR use on nurses’ workflow interruption and mental workload [12]. Although EMR is an important tool for documenting hospital records, it is important to recognize that it contributes to the stress of nurses who use it. The challenge is to address these stressors, and efforts should be made to optimize EMR on the basis of evidence and strategies based on user experience.
In Korea, the Electronic Health Record (EHR) was first introduced in 2003, and it was a system that included both inpatient and outpatient care at tertiary hospitals. As of 2024, Korean hospitals are using a considerably advanced form of EMR, but the specific introduction and use of EMR are not well known. Accordingly, Cho et al. [13] stated that it is necessary to investigate the current status of ENR application used by Korean nurses and that since the advantages and disadvantages of ENR have been reported, a qualitative study is needed on the experience of Korean nurses using the ENR.
In this way, previous studies have investigated the experience of using ENR among nurses and reported ways to improve the use of ENR and work performance based on the experiences and perceptions of nurses. However, in Korea, although ENR has been steadily developing since its introduction, there has been no report on the experience of using ENR experienced by nurses, who are the main users, over the past 10 years.
Therefore, this study aimed to qualitatively and explanatively investigate the experiences of nurses using ENR in frontline settings with high acuity and high infection risk, such as emergency departments and intensive care units, where ENR support is more critical than other clinical settings in the post-pandemic era.
METHODS
Study design
This study was a qualitative descriptive study aimed at exploring nurses’ experiences of using the ENR.
Participants
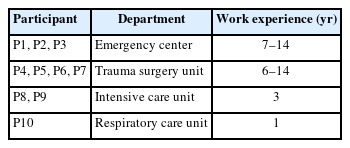
Study participants were 10 nurses who had been working for more than 6 months at the tertiary hospital in Korea. They are nurses working in acute wards such as emergency rooms, intensive care units, and medical/surgical intensive care units, which are frontline environments with a high risk of infection after the pandemic. Informed consent was obtained through approval by hospital and department administrators. Department administrators provided contact information for potential participants (Table 1).
Data collection
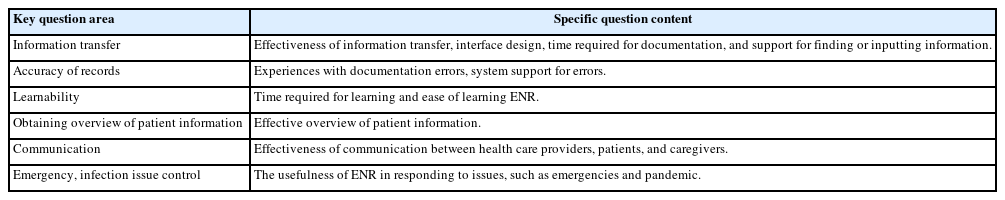
The data collection period was from September 2023 to February 2024. Interviews were conducted in the form of individual in-depth interviews, based on semi-structured questions prepared in advance by the researchers. The interview questions were prepared based on previous studies. The questions included six key areas: ‘information transfer,’ ‘accuracy of records,’ ‘learnability,’ obtaining overview of patient information,’ ‘communication,’ and ‘emergency, infection issue control.’ Examples of specific questions for each area include the following (Table 2). Data collection and analysis were conducted simultaneously. After interviewing 10 participants, it was determined that data saturation had been reached as no new themes emerged. Therefore, statements from 10 participants were included in the analysis.
Data analysis
The analysis was conducted according to Downe-Wamboldt’s content analysis [14]. The researcher thoroughly listened to and read the interview data more than five times to gain a solid understanding of the data. During the thorough reading process, the researcher initially identified five subjects: system, user (organization), user (individual), positive factors, and negative factors. The analysis was conducted using Microsoft Excel. The initial coded data were revised through a researcher meeting and integrated into three subjects: system, positive factors, and the user through a process of grouping similar categories. To ensure the validity of this analysis, it was reviewed by a nursing scholar with experience in qualitative research. Ultimately, three subjects (‘improvements to ENR implementation,’ ‘benefits of ENR implementation,’ and ‘ENR user factors’), five categories, and eight subcategories were derived.
Trustworthiness
To ensure the trustworthiness of the research, the four aspects proposed by Guba [15] were considered. To ensure the credibility, three researchers debriefed the data and received feedback from two participants and one nursing scholar. To ensure the dependability, Microsoft Excel was used for data management, and the analysis, including the initial coding, was conducted systematically. To ensure transferability, the roles of the researchers, the methods for participant recruitment and data collection, and the data analysis procedures were detailed explicitly. To ensure the confirmability, the findings were reviewed by two participants and one nursing scholar.
Ethical consideration
Institutional review board (IRB) approval (IRB No: 1044396-202309-HR-178-01) was obtained from the IRB of the Gachon University to which the researcher is affiliated.
RESULTS
We identified three subjects, five categories, and eight subcategories. The subjects were: ‘improvements to ENR implementation,’ ‘benefits of ENR implementation,’ and ‘ENR user factors.’ Under ‘improvements to ENR implementation,’ the categories were ‘information finding and sharing function’ and ‘information input function.’ The subject of ‘benefits of ENR implementation’ included ‘facilitating efficient communication’. Lastly, ‘ENR user factors’ had the categories of ‘ensuring record quality’ and ‘need for education’ (Table 3).
Improvements to electronic nursing record implementation
Two categories were derived in this area: ‘information finding and sharing function’ and ‘information input function’.
Information finding and sharing function
Participants emphasized the necessity of developing specialized interfaces, such as pop-up screens, to facilitate the efficient finding and sharing of critical information, including infection and emergency data as well as patient-specific details.
Special screens (e.g., pop-ups) for easy sharing specific information
(For isolated patients) It would be useful to have a pop-up screen indicating that procedures need to be performed in a negative pressure room. (P 3) Sharing special patient details in ENR is challenging; For example, other departments often have a hard time finding urgent behavior issues for patients flagged in the ENR. (P 1)
Information input function
Concerning input functionality, the necessity for mechanisms to detect errors—including typographical and biometric input errors—was emphasized. Additionally, addressing system instabilities such as duplicate entries, redundant links, and automatic deletions was identified as a critical priority. Furthermore, it was underscored that templates should be designed to better accommodate nursing workflows, ensuring that data collected by nurses, such as photographs, are accurately recorded in nursing records rather than in physician records.
Identifying documentation errors (alarms and warnings)
The ENR has no typo detection, so we must manually check for typos and errors may remain. It would be helpful if there were warnings or notifications (alarms) for typos. (P 7, 9)
Input system instability (duplicate entry and redundant links, automatic deletion)
System instability causes items to be entered twice into nursing records, disrupting my work and requiring me to delete them individually. (P 5) ENR requires extensive input, and missing even one entry results in all records being deleted, forcing me to start over, which is very disruptive to my work. (P 3)
Need for nursing-friendly templates
In ICUs, we document in both the cardex and the ENR. Having a cardex template would eliminate the need for double-recording and reduce overtime work caused by this duplication. (P 2) There are insufficient checkboxes for nursing needs, resulting in excessive text entry. Nursing checkboxes need further development. (P 7) The current ENR lacks support for photographic records, forcing me to enter the doctor’s name in their record, which is problematic. (P 1, 8)
Benefits of electronic nursing record implementation
In this area, one category was derived: ‘facilitating efficient communication’.
Facilitating efficient communication
Participants stated that using ENR helps in ‘effective communication among medical staff’, and that ‘visualizing specific information’ (e.g., COVID-19 confirmed case notification screen, handover screen, drug-specific information display function) is useful in communicating specialized information.
Efficient communication among medical staff
Physicians review ENR in detail and often request additional information or suggest adding details to nursing records. The ENR enhances communication between medical staff and improves job performance. (P 1, 6)
The usefulness of visualization of specific information
The EMR now includes a COVID-19 patient alert screen, which is quick and easy to check in emergency settings. (P 2) Screens like ‘Clinical Observation’ and ‘Nursing Progress’ on the handover screen provide a quick overview of the patient’s condition. (P 6) If a patient has a drug allergy, an indicator next to the drug name appears when prescribed, allowing for a double-check before administration. This is very helpful. (P 4)
Electronic nursing record user factors
In this area, two categories were derived: ‘ensuring record quality’ and ‘need for education’. Participants stated that user factors should also be considered for the use of ENR to bring efficiency and satisfaction to nursing work.
Ensuring record quality
Participants noted that while the ENR enhances recording efficiency, its accuracy is frequently compromised by user practices. For instance, ENR tends to favor hospital-centered records over patient-centered ones due to factors such as hospital audits, resulting in inaccurate patient information. Additionally, although the C&P function is useful, its widespread misuse—such as copying incorrect information and omitting details—further undermines record accuracy.
Demand for accurate patient information records
Nursing records often affected by hospital assessments, which makes us leave out patient details that could cause problems at the hospital level. This leading to EMR records less accurate. (P 1) Copy-pasting often lowers the quality of documentation. While copying can be useful, we often just paste without adding detailed notes when we’re busy. We also sometimes skip editing after copying and just copy again, leading to inaccurate records. Users need to be aware of this issue. (P 3, 6)
Need for education
Nurses using ENR reported a lack of support for learning ENR. Nurses emphasized that more systematic education should be provided at the institutional level.
Systematic electronic nursing record learning support
When we started working in hospitals, there was little training or resources for the ENR. We got just 1 day of training and had to figure it out ourselves. Hospitals don’t offer systematic ENR training, and it looks like many features aren’t being used properly. (P 1, 5)
DISCUSSION
Through the analysis of hospital nurses’ experience of using ENR, we identified three subjects: improvements to ENR implementation, benefits of ENR implementation, and ENR user factors.
Regarding ‘improvements to ENR implementation,’ participants indicated that both the information finding and sharing function and the information input function need to be enhanced. Participants suggested that the ENR’s information finding and sharing function should be improved to enable rapid sharing of special information such as negative pressure room situations and patient-specific information in infection and emergency situations. In special situations such as emergencies and pandemics, the roles of personnel, equipment, and beds are extremely important. It is crucial to be able to respond immediately and in real-time according to the severity of the patient’s condition [16]. Participants suggested enhancing the ENR with information-sharing interfaces, like ‘pop-up’ or ‘single screens,’ to enable quick sharing of resource status and patient-specific information for timely and effective responses. Research related to the optimization of EHR usability emphasizes the importance of developing interfaces that capture clinical workflows. To achieve this, collaboration between developers and users is paramount, and nurses’ experiences must be incorporated into ENR development [17].
Additionally, participants indicated that the information input functions of the ENR need to be enhanced in various ways. Participants pointed out that they must manually check for errors in ENR, which is time-consuming and burdensome, and errors sometimes go unnoticed. As it may compromise the accuracy of the records, this requires a feature that can identify typos, such as warnings and notifications. Another problem is that the system’s connection function is unstable, which causes duplicate connections, forcing nurses to manually check each document. This not only delays nursing work but also increases the workload and burden on nurses. Therefore, it appears that system improvement is necessary to stabilize unstable input functions such as automatic double entry, duplicate linking, and automatic deletion.
Also, participants pointed out that more nurse-friendly templates should be designed to support nursing work efficiently. For example, the cardex is a template that nurses have used for a long time, but the ENR does not support this function. As a result, nurses were using it manually and performing redundant tasks by recording the cardex content in the ENR as well. Double documentation leads to delays in work and reduces efficiency, causing overtime for nurses, which negatively impacts both nurses and patients [18]. Therefore, it is essential to minimize this double documentation. Although some may perceive nurses’ attachment to their preferred methods as a barrier to ENR adoption [19], if these methods are consistently favored by the nurses, it becomes crucial to thoughtfully integrate them into the nursing workflow. Furthermore, the fixed input method also presents inefficiencies, as it lacks sufficient nursing-related options. Participants pointed out that tasks that could be easily handled with checkboxes often have to be entered as text, leading to inefficiency in their work.
Another issue reported is that there is no photo-saving function on the nursing record screen, so nurses save photos on the physician's record screen. This current practice of documenting nursing records under the name of the physician reduces the reliability of medical records. This also has legal implications [20], so the input function for nursing records should be improved to allow documentation under the name of the performing nurse. These issues indicate the lack of user-friendliness of the current ENR for nursing tasks. Lack of user-friendliness is directly related to the accuracy of documentation, time efficiency, and overall nursing workload, and the inefficient workflow is a major obstacle to the effective use of the ENR [19,21]. Previous studies have identified issues such as the lack of routine input functions (such as photos) and problems with record linking functions as “factors that interfere with routine nursing workflows” [22]. Ting et al. [22] emphasized that the continuous involvement of nurses in the development of ENR is essential to address these issues. Therefore, it is crucial to continuously improve the ENR to function as a nurse-friendly platform that matches the nursing workflow.
Meanwhile, participants mentioned efficient communication between physicians and nurses as the ‘benefits of ENR implementation.’ Nurses reported that ENR not only provides a comprehensive view of patient information and data integration, but also promotes integrated clinical communication between physicians and nurses. Nurses managing emergency and infection issues emphasized that functions visualizing special information, like the COVID-19 notification screen, “clinical observation” and “nursing progress” interfaces, and drug-specific displays, help facilitate communication. Notifications and alerts are valuable functions of EMR that support decision-making by medical staff. The visual design of the EMR interface has been reported to have a direct impact on patient care and safety [21], and this effectively facilitates communication between medical staff [23]. Since high-quality ENR significantly affects treatment outcomes [24], it is important to study optimizing ENR so that the benefits of ENR are reflected in nursing workflow [21]. We suggest conducting further research to enhance the benefits of ENR in optimizing and supporting nursing workflow.
Participants also reported that ‘ENR user factors’ should be considered. First, participants emphasized that ensuring the quality of ENR records is important and that this requires user reflection. In terms of record quality, participants expressed concerns that nursing records are shifting toward meeting hospital evaluation criteria (rather than being patient-centered). This is consistent with the criticism that hospitals tend to prioritize institutional policies, which in turn shifts the focus of documentation from patient-centered to institutional priorities [25]. Dillard-Wright [26] also noted that nursing has shifted to a task-centered approach due to EHR implementation, which has reduced nurses’ critical thinking competencies. However, given the reality that nursing and documentation in the ENR environment are often determined by the financial interests of the hospital [27], it is difficult for nurses to address this issue on their own. Therefore, as ENR users, nurses should strive to identify and conduct research on factors that threaten the quality of nursing documentation and patient-centered records.
In addition, the C&P function has been pointed out as an obstacle to the accurate recording of ENR. Recent studies report that users commonly rely on the C&P function to reduce EMR recording time, but concerns arise about declining record quality due to indiscriminate use, leading to errors and the repeated distribution of incorrect data [5,10,21], which can spread inaccuracies. Therefore, EMR users should consider user factors (e.g., workload and time pressure) that affect the quality of records using C&P, and it is essential to establish and adhere to C&P usage principles [10]. In other words, it is necessary to adjust ‘user awareness and environment’ so that the convenient C&P function of ENR does not lead to incomplete records.
Finally, participants indicated that on-site training for ENR was insufficient. In particular, nurses emphasized the need for systematic and sufficient ENR learning support early in their careers. A lack of ENR training threatens users’ ability to effectively use the ENR and consequently reduces the quality of nursing records [28]. Ting et al. [22] recommended various ENR training strategies, such as eLearning, peer coaching, simulation training, involving clinical nurses in education, and aligning training with nurses’ clinical workflows. The insufficiency of ENR training currently provided in the Korean clinical environment should be reconsidered.
Based on the above discussion, some recommendations can be made for the research and educational aspects. First, in terms of research, it is essential to conduct research that actively integrates nurses as the main ENR users to ensure that nursing workflows are adequately reflected. In addition, research is needed to ensure that the ENR reflects the daily nursing workflow and becomes a more friendly platform for nurses. Second, in terms of education, it is important to implement sufficient and effective educational strategies to improve ENR application skills and prevent the deterioration of nursing documentation quality. Furthermore, research is needed to identify factors that threaten patient-centered records and develop strategies to control these influencing factors to ensure the quality of ENR documentation.
In conclusion, although our results demonstrate that ENR use improves the nursing work environment and quality of care, there is still room for improvement in both ENR functionality (e.g., recording and sharing capabilities) and user factors. We hope that the findings of this study will provide a foundation for further optimizing the ENR to better support nursing workflow and advance nursing practice.
Notes
AUTHOR CONTRIBUTIONS
Dr. Hee Jung KIM had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors reviewed this manuscript and agreed to individual contributions.
Conceptualization: all authors. Methodology: all authors. Investigation: all authors. Data curation: all authors. Formal analysis: all authors. Writing–original draft: YHL and MSK. Writing–review & editing: HJK.
CONFLICTS OF INTEREST
No existing or potential conflict of interest relevant to this article was reported.
FUNDING
None.
DATA AVAILABILITY
Due to privacy concerns, the data underlying this study cannot be made publicly available. Requests for data access may be directed to the corresponding author.
ACKNOWLEDGMENTS
We appreciate all the study participants for their contributions.