| Korean J Health Promot > Volume 24(3); 2024 > Article |
|
ABSTRACT
Background
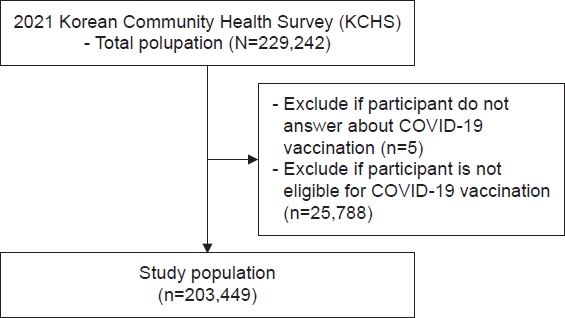
Methods
Results
Conclusions
AUTHOR CONTRIBUTIONS
Dr. Sung SUNWOO had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors reviewed this manuscript and agreed to individual contributions.
Conceptualization: YHL and SEP. Data curation: YHL and SEP. Formal analysis: YHL and SEP. Investigation: YHL. Methodology: YHL. Software: YHL. Validation: YHL. Writing–original draft: YHL. Writing–review & editing: SS.
CONFLICTS OF INTEREST
No existing or potential conflict of interest relevant to this article was reported.
Table 1.
Table 2.
Table 3.
Table 4.
REFERENCES
-
METRICS

-
- 1 Crossref
- 0 Scopus
- 1,281 View
- 13 Download
- ORCID iDs
-
Yong Ho LEE

https://orcid.org/0000-0001-5056-6393Seong-Eon PARK

https://orcid.org/0000-0001-9224-2979Sung SUNWOO

https://orcid.org/0000-0002-0521-4804 - Related articles

 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


