Association between Allergic Rhinitis and Osteoarthritis in the Korean Adult Population-Based on the 3rd to 8th Korea National Health and Nutrition Examination Survey
Article information
Abstract
Background
Recent studies reported a significant association between asthma and osteoarthritis, but the relationship between allergic rhinitis and osteoarthritis has not been studied sufficiently. This study aimed to determine the association between allergic rhinitis and osteoarthritis in adults.
Methods
Using data from the 3rd to 8th Korea National Health and Nutrition Examination Survey, multiple logistic and linear regression analyses were conducted to determine the association between allergic rhinitis and osteoarthritis with adjustment for potential confounding factors in participants aged 50 years or older.
Results
When adjusted for potential confounders, doctor-diagnosed osteoarthritis (adjusted odds ratio [OR]=1.32, 95% confidence interval [95% CI] =1.12–1.57, P=0.001), knee pain (adjusted OR=2.42, 95% CI=1.32–4.41, P=0.004), and symptomatic knee osteoarthritis (adjusted OR=2.69, 95% CI=1.10–6.57, P=0.030) were all significantly more frequent in participants with allergic rhinitis than in those without it.
Conclusions
These findings show an evident association between allergic rhinitis and osteoarthritis in Korean adults.
INTRODUCTION
Osteoarthritis is a common degenerative joint disease that causes pain and structural and functional damage [1]. The pathogenesis of osteoarthritis is largely unknown, and there is no treatment method to restore damaged cartilage or slow down the progression of the disease [2]. Recently, it has been reported that immunoglobulin E (IgE)-mediated activation of mast cells in the synovium may play an important role in driving the progression of osteoarthritis [3]. The IgE-mediated degranulation of mast cells is also a characteristic of allergic diseases, and recent studies have shown a genetic association between osteoarthritis and allergic diseases such as asthma and allergic rhinitis [4]. If molecular pathways related to allergic conditions play a key role in the mechanism of osteoarthritis, therapeutic agents targeting them might prevent the development or progression of osteoarthritis. A retrospective cohort study reported that the risk of developing osteoarthritis is increased in patients with asthma or atopic dermatitis [5]. A significant association between asthma and osteoarthritis was also reported in a cross-sectional study conducted in Korea [6]. On the other hand, a Japanese study revealed ambiguous results, showing that osteoarthritis of the temporomandibular joint was not related to asthma, but related to allergies [7]. In addition, Korean studies using data from the Korea National Health and Nutrition Examination Survey (KNHANES) reported conflicting results regarding the relationship between allergic rhinitis and osteoarthritis [8,9]. However, both studies used only 3 to 4 years of the KNHANES data and included the entire population aged 19 or older [8,9]. As a result, the majority of the study subjects were in the age group where osteoarthritis is not prevalent [8,9]. Thus, this study aimed to investigate the relationship between allergic rhinitis and osteoarthritis among participants aged 50 years or older in the KNHANES from the 3rd to the 8th period.
METHODS
Study population
This study was conducted using data from the KNHANES from 2005 to 2021. The survey includes a health interview, physical examination, and laboratory tests. In 2005 to 2021, the KNHANES collected data on doctor-diagnosed osteoarthritis. In 2010 to 2013, the KNHANES included a screening survey for knee osteoarthritis. Accordingly, this study analyzed two study populations: study population 1 to confirm the association between allergic rhinitis and doctor-diagnosed osteoarthritis and study population 2 to confirm the association between allergic rhinitis and outcomes from the screening survey for knee osteoarthritis.
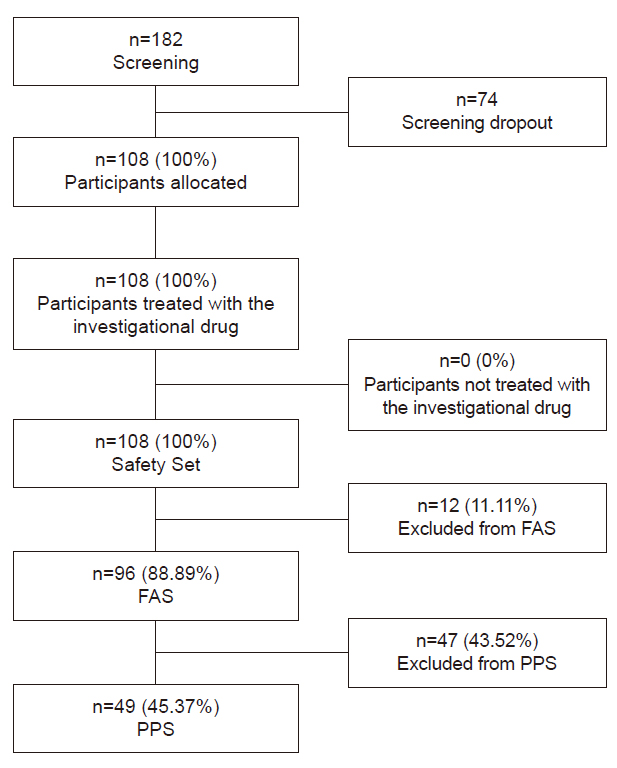
Study population 1 consisted of participants from 2005 to 2021. Because the prevalence of osteoarthritis is very low under 50 years of age, and the screening survey for knee osteoarthritis was conducted in participants aged 50 years or older, subjects younger than 50 years were excluded. In addition, the following subjects were excluded subsequently: those with missing data on doctor-diagnosed osteoarthritis and allergic rhinitis, and those with incomplete data on potential confounding variables. Thus, a total of 44,538 subjects were included in study population 1 (Fig. 1). Additionally, subjects without data on the screening survey for knee osteoarthritis were excluded from study population 1, and the remaining 10,729 subjects were designated as study population 2 (Fig. 1).
Variable definitions
The doctor-diagnosed osteoarthritis was determined by the following question: “Have you been diagnosed with osteoarthritis by a doctor?” [6] Allergic rhinitis was determined by whether or not the participant was diagnosed by a doctor before the age of 50. Knee pain was determined by the following question: “Have you had knee pain for 30 days or longer in the past 3 months?” If “yes”, the respondents were asked the average degree of pain on a scale of 0 to 10 regardless of medication use. If “no”, the knee pain score was considered as 0. The osteoarthritis screening survey included radiographic examination of the knee (SD3000 Synchro Stand; Accele Ray, Bern, Switzerland) [6]. Radiographic knee osteoarthritis was defined as a Kellgren-Lawrence Grading Scale score ≥2 [10]. Symptomatic knee osteoarthritis was defined as having both radiographic knee osteoarthritis and knee pain [11].
Age was classified as 50 to <60 years, 60 to <70 years, and 70 years or older. Education level was divided into elementary school or less, middle school, high school, and college or above. Household income was divided into four groups according to income quartile: low, mid-low, mid-high, and high. Occupation was classified based on Korean Standard Classification of Occupations as follows: group 1 (managers, professionals, and related workers); group 2 (clerks); group 3 (service and sales workers); group 4 (skilled agricultural, forestry, and fishery workers); group 5 (craft, equipment, and machine operating and assembling workers); group 6 (elementary workers); and group 7 (housewives, students, and the unemployed). In this study, groups 1, 2, 3, and 7 were merged into a single group (Group A) and groups 4, 5, and 6 were also merged (Group B) [12]. Smoking was classified as never smoked, ex-smoker, current smoker: those who smoked less than 100 cigarettes in their lifetime defined as never smoked, those who smoked in the past but do not currently smoke defined as ex-smokers, and those who currently smoked defined as current smokers [13].
Statistical analyses
Because the KNHANES used a multi-stage stratified cluster probability sampling method, the clusters, strata, and weights of the data were used to account for the complex sampling design. All statistical analyses were conducted using the statistical software package R version 4.2.3 (The R Foundation for Statistical Computing), and a two-sided P-value less than 0.05 was considered as statistically significant.
The proportions or means and standard deviations were estimated for demographic, socioeconomic, and clinical variables. The differences in the variables according to doctor-diagnosed osteoarthritis or allergic rhinitis were assessed using the Pearson chi-square test with Rao-Scott adjustment or design-based Wilcoxon rank-sum test for complex sample survey data.
To estimate odds ratios (ORs) of doctor-diagnosed osteoarthritis according to allergic rhinitis in study population 1, simple and multiple logistic regression analyses were performed. The multiple logistic regression model included potential confounding variables such as sex, age, education, household income, occupation, smoking, and body mass index.
To estimate ORs of knee pain, radiographic knee osteoarthritis, and symptomatic knee osteoarthritis according to allergic rhinitis in study population 2, simple and multiple logistic regression analyses were also conducted. The multiple logistic regression models included the same confounding variables as those used in study population 1.
To estimate the mean knee pain scores according to allergic rhinitis in subjects with radiographic knee osteoarthritis, simple and multiple linear regression analyses were conducted. The multiple linear regression models included the same confounding variables as those used in the multiple logistic regression models.
Ethics statement
This study was exempted from approval by the Institutional Review Board because this study was a secondary data analysis of existing data.
RESULTS
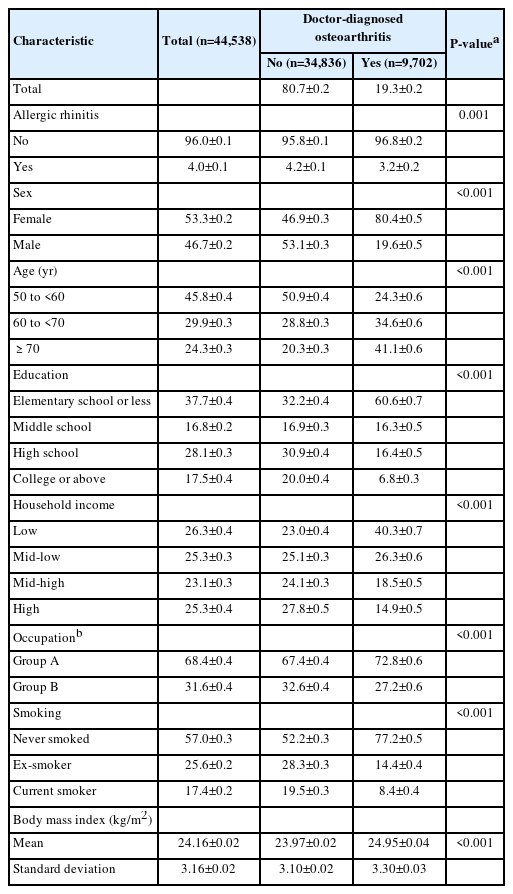
The demographic, socioeconomic, and clinical characteristics of study population 1 are summarized in Table 1. The frequency of allergic rhinitis was lower in subjects with doctor-diagnosed osteoarthritis than in those without it (proportion±standard error, 3.2%±0.2% vs. 4.2%±0.1%; P=0.001).
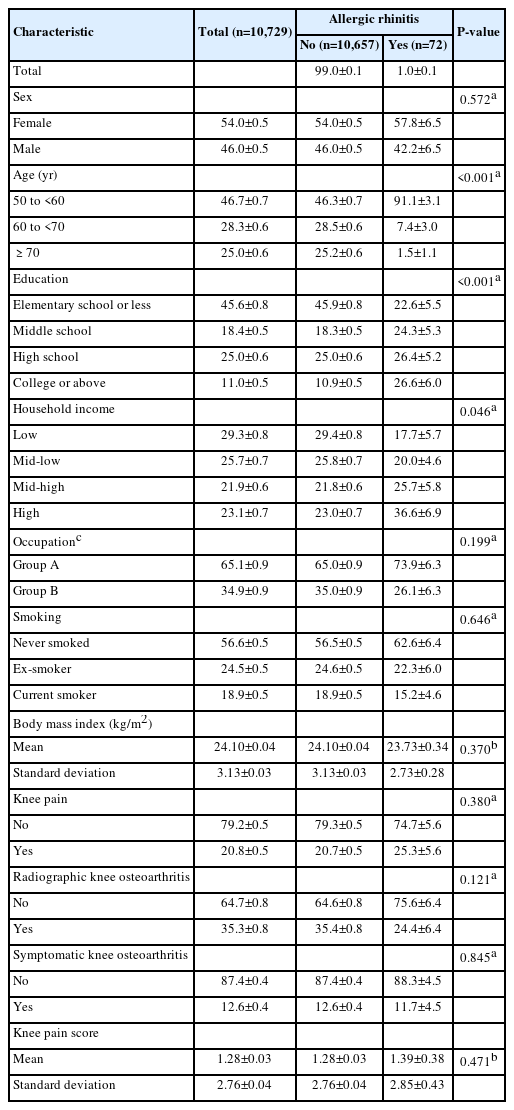
The characteristics of study population 2 are presented in Table 2. There was no significant difference in the frequencies of knee pain, radiographic knee osteoarthritis, and symptomatic knee osteoarthritis between those with and without allergic rhinitis (P=0.380, 0.121, and 0.845, respectively). Knee pain scores were also not significantly different between those with and without allergic rhinitis (P=0.471).
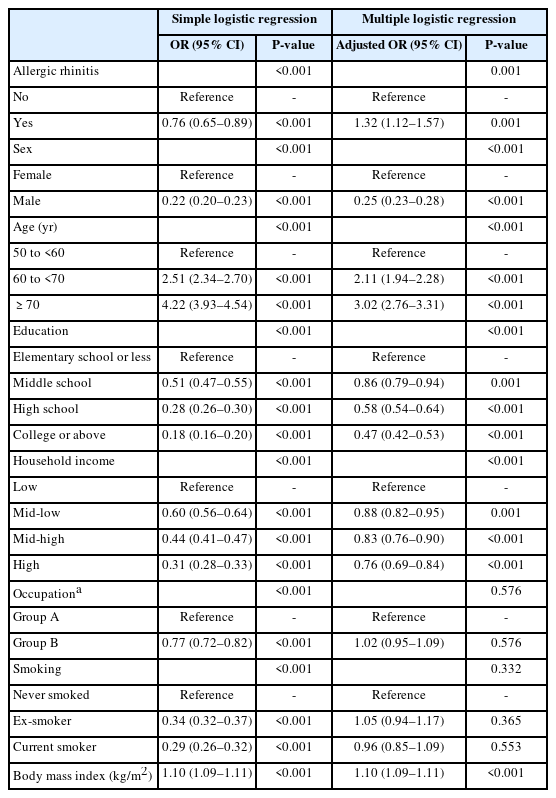
Without adjustment for potential confounders, the odds of doctor-diagnosed osteoarthritis were significantly lower in subjects with allergic rhinitis than in those without it (OR=0.76, 95% confidence interval [95% CI]=0.65–0.89, P<0.001) (Table 3). However, the multiple logistic regression analysis adjusting for confounding factors showed that the odds of doctor-diagnosed osteoarthritis were significantly higher in participants with allergic rhinitis than in those without it (adjusted OR=1.32, 95% CI=1.12–1.57, P=0.001) (Table 3).
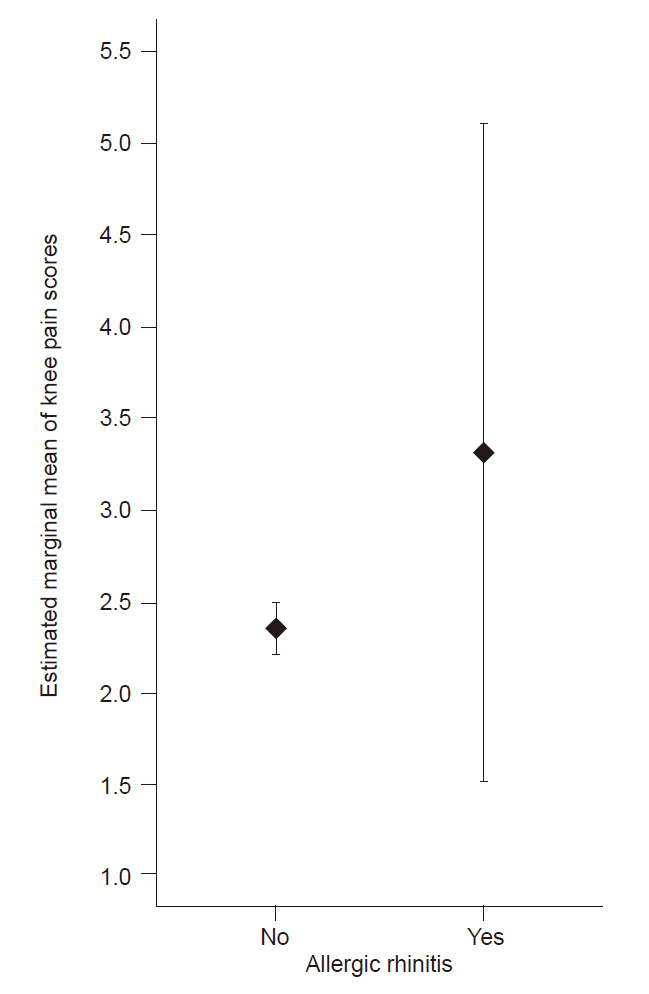
Without adjustment for confounders, the odds of knee pain were not significantly different between subjects with and without allergic rhinitis (OR=1.30, 95% CI=0.72–2.33, P=0.381) (Table 4). However, multiple logistic regression analyses adjusting for confounders showed that the odds of knee pain were significantly higher in participants with allergic rhinitis than in those without it (adjusted OR=2.42, 95% CI=1.32–4.41, P=0.004) (Table 4).
Association of allergic rhinitis with knee pain, radiographic knee osteoarthritis, and symptomatic knee osteoarthritis in study population 2
The odds of radiographic knee osteoarthritis were not significantly different between subjects with and without allergic rhinitis regardless of adjustment for confounders (P=0.126 and 0.458 for without and with confounder adjustment, respectively) (Table 4).
Without adjustment for confounders, the odds of symptomatic knee osteoarthritis were not significantly different between subjects with and without allergic rhinitis (OR=0.92, 95% CI=0.40–2.14, P=0.846) (Table 4). However, multiple logistic regression analyses adjusting for confounders showed that the odds of symptomatic knee osteoarthritis were significantly higher in participants with allergic rhinitis than in those without it (adjusted OR=2.69, 95% CI=1.10–6.57, P=0.030) (Table 4).
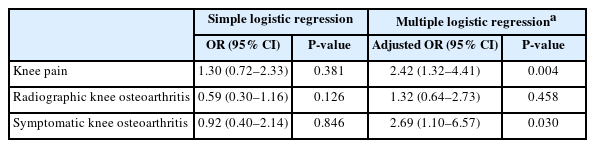
Without adjustment for confounders, mean knee pain scores were not significantly different between participants with and without allergic rhinitis (P=0.710) (Table 5). When adjusted for confounders, mean knee pain scores were also not significantly different between participants with and without allergic rhinitis (estimated marginal means 3.31 [95% CI=1.51–5.11] vs. 2.35 [95% CI=2.21–2.48], respectively; adjusted mean difference 0.96 [95% CI=–0.84 to 2.77], P=0.295) (Table 5, Fig. 2).

Association of allergic rhinitis with knee pain scores in participants with radiographic knee osteoarthritis
DISCUSSION
The results of this study show that there is an evident association between allergic rhinitis and osteoarthritis. When adjusted for potential confounders, doctor-diagnosed osteoarthritis, knee pain, and symptomatic knee osteoarthritis were all significantly more frequent in participants with allergic rhinitis. To the best of my knowledge, there have been no large-scale studies that investigated the relationship between allergic rhinitis and osteoarthritis in particular with analysis on the pain and radiographic findings of specific joints. Additionally, since the KNHANES data used in this study are nationally representative, the findings of this study can be extrapolated to the general Korean adult population aged 50 years or older.
There have been few studies on the relationship between allergic rhinitis and osteoarthritis, and their results were inconsistent, making it difficult to reach a clear conclusion. An et al. [8] analyzed the KNHANES data from 2008 to 2011 and reported that there is no significant association between allergic rhinitis and osteoarthritis. On the other hand, Lee et al. [9] reported that osteoarthritis is more prevalent in those with allergic rhinitis by analyzing the KNHANES data from 2016 to 2018. Both studies covered only 3 to 4 years of the KNHANES data, and neither of the studies analyzed symptoms and radiographic findings for the knee joint. Accordingly, this study covered a total of 16 years of KNHANES data from the 3rd to the 8th period, and analyzed the osteoarthritis screening survey data from 2010 to 2013 as main outcome variables.
The association between allergic rhinitis and osteoarthritis may result from the genetic link between the two diseases. A recent study showed that those with genetic variations associated with allergic rhinitis and asthma have an increased risk of developing osteoarthritis [4]. It has also been reported that increased serum IgE levels are associated with osteoarthritis of the knee [14]. IgE may contribute to the aggravation of osteoarthritis by activating mast cells in the synovium [3]. An increase in serum IgE levels is also common in allergic conditions including allergic rhinitis, asthma, and atopic dermatitis, which might contribute to the association between osteoarthritis and the allergic conditions. Further studies would be needed to elucidate the underlying mechanisms.
The results of this study show that the adjustment for confounding variables was necessary to confirm the association between allergic rhinitis and osteoarthritis. Without adjusting for confounding factors, no significant association or even an inverse relationship was found between allergic rhinitis and osteoarthritis. However, when adjusting for confounding variables, the significant associations were confirmed between allergic rhinitis and osteoarthritis. This appears to mainly result from the confounding effect of age. The prevalence of osteoarthritis increased rapidly with age, but that of allergic rhinitis showed the opposite pattern.
In contrast with doctor diagnosis of osteoarthritis, knee pain, and symptomatic knee osteoarthritis, radiographic knee osteoarthritis was not more frequent in those with allergic rhinitis. The cause of this difference between clinical and radiological findings is unclear, but it is known that radiographic diagnosis of osteoarthritis is often discordant with clinical symptoms [15]. Thus, the diagnosis of osteoarthritis is based on clinical symptoms and signs as well as radiological findings [16], and patient’s symptoms may be more meaningful related to the functional outcomes than radiological findings [17]. Furthermore, the Kellgren-Lawrence Grading Scale has been criticized on the basis of its reliability and the lack of recognition of patellofemoral arthritis [18]. When conducting epidemiological studies on osteoarthritis, one of three definitions of osteoarthritis is commonly used: subjects’ self-reports, radiographic osteoarthritis, or symptomatic osteoarthritis [11]. Generally, the radiographic definition leads to higher prevalence and heterogeneous results between studies. In contrast, subjects’ self-reports and symptomatic osteoarthritis result in similar prevalence estimates and show more homogeneous and consistent results across studies [11]. On the other hand, allergic rhinitis may play a role in aggravating symptoms of osteoarthritis rather than initiating the disease. Activated mast cells are known to aggravate pain in joints with osteoarthritis and their number in the synovium has a positive correlation with the disease severity [19]. The increase in IgE, which is common in allergic rhinitis, induces mast cell activation. These mechanisms might underlie the worse osteoarthritis symptoms in subjects with allergic rhinitis observed in this study.
Among subjects with radiographic knee osteoarthritis, the mean knee pain score was numerically higher in participants with allergic rhinitis than in those without it, but the difference was not statistically significant. This statistical insignificance appears to be due to insufficient statistical power from the small number of subjects available for the analyses. Because the linear regression analyzed only subjects with radiographic knee osteoarthritis, not the entire study population 2, the number of subjects was inevitably small compared to the other analyses.
This study has several limitations. First, the cross-sectional design of the KNHANES made it possible to determine the association between allergic rhinitis and osteoarthritis, but additional studies will be needed to confirm the causality between them. Second, doctor diagnoses of osteoarthritis and allergic rhinitis may be inaccurate as they were based solely on participant reports. Third, because the KNHANES was conducted within Korea, it is difficult to directly extrapolate the results of this study to other countries.
In conclusion, this study confirmed a clear association between allergic rhinitis and osteoarthritis in Korean adults. Further studies will be needed to determine whether this association is generally observed in other populations and whether a causal relationship also exists between them.
Notes
AUTHOR CONTRIBUTIONS
Dr. Sunmi KIM had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Sunmi KIM reviewed this manuscript and agreed to individual contributions.
Conceptualization, Data curation, Formal analysis, Methodology, Software, Writing–original draft, Writing–review & editing: SK.
CONFLICTS OF INTEREST
No existing or potential conflict of interest relevant to this article was reported.
FUNDING
None.
DATA AVAILABILITY
The data presented in this study are available upon reasonable request from the corresponding author.