| Korean J Health Promot > Volume 16(3); 2016 > Article |
|
ABSTRACT
Background
Korea has high prescribing rate and rising antibiotic resistance. This study was conducted to understand why primary physicians prescribe antibiotics for acute respiratory infections and to explore the factors that influence antibiotic resistance, and so to suggest strategy to reduce antibiotic resistance.
Methods
A qualitative exploratory approach was used using 4 focus groups composed of physicians from different area. A semi-structured guide was applied in obtaining the physicians' opinions. Common themes were extracted by authors, which were used to gather results and draw conclusion.
Results
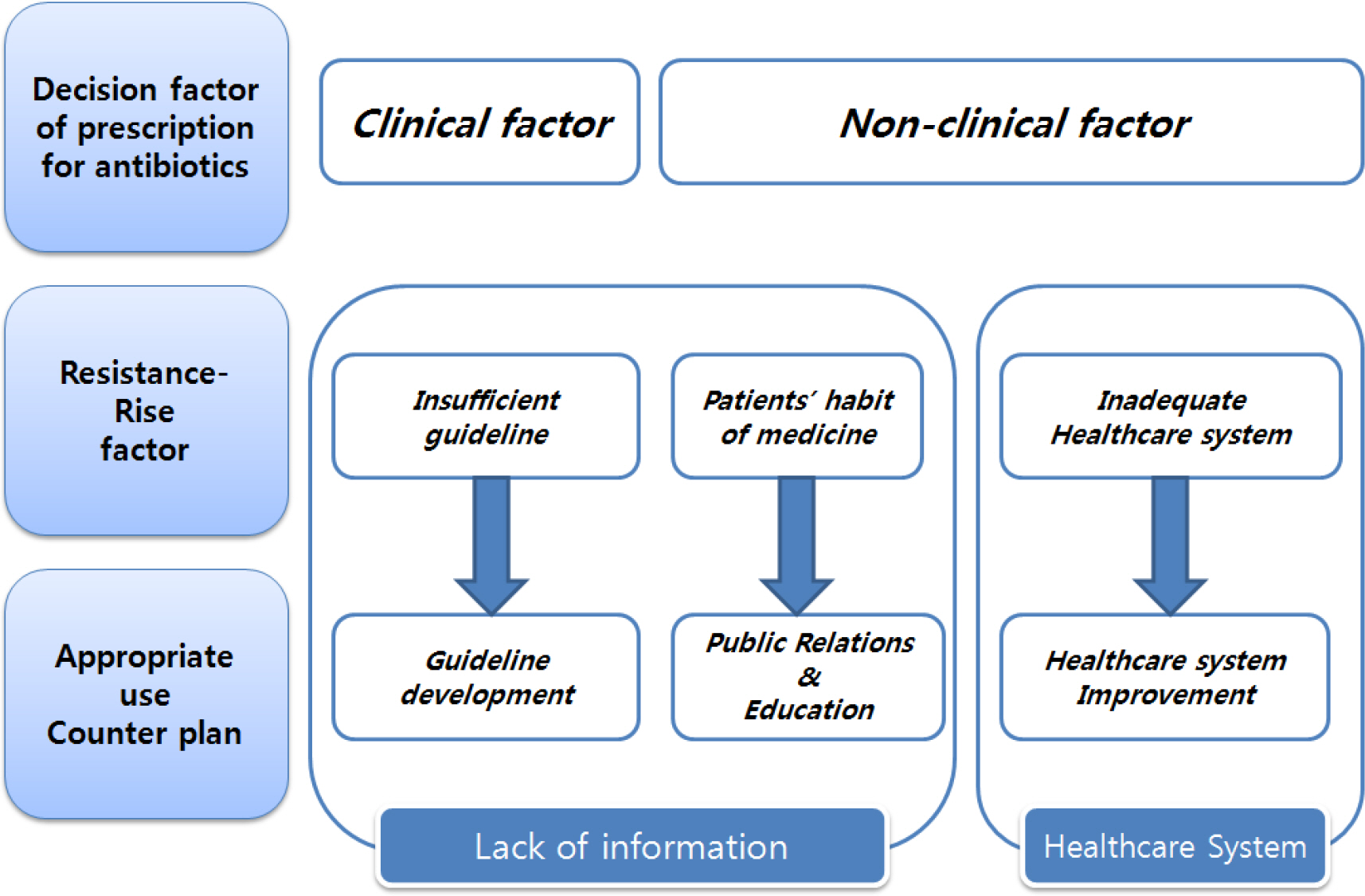
Participants acknowledged multiple factors such as clinical factor and competitive environment are involved in physicians' decision of antibiotic prescribing. They identified that causes of rising antibiotic resistance were shortage of information, discontinuation of taking antibiotics, and other system factors.
Conclusion
Participants were certain that less prescribing antibiotics and selecting appropriate antibiotics might be method to reduce antibiotic resistance. To change the prescribing behavior, it should be provided periodically for community physicians with prescribing information and specific guidelines for antibiotics resistance. Patients should be also noticed about antibiotic medication information more accurately. Including prescription incentive policy, improvement of healthcare system will be carried out at the same time.
Table┬Ā1.
Interview participants
References
1. World Health Organization. Antimicrobial Resistance Global Report on Surveillance 2014. Geneva: World Health Organization; 2014.
2. McCaig LF, Besses RE, Hughes JM. Antimicrobial drug prescription in ambulatory care settings, United States, 1992ŌĆō2000. Emerg Infect Dis 2003;9(4):432-7.



3. McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA 1995;273(3):214-9.


4. Center for Disease Prevention and Control. National Diabetes Fact Sheet [Internet]. Atlanta: Center for Disease Prevention and Control; 2005. [Accessed September 26, 2016]. Available from:. http://www.cdc.gov/media/pressrel/2007/r071016.htm.
5. Song JH, Joo EJ. The crisis of antimicrobial resistance: current st atus and future strategies. Korean Med Assoc 2010;53(11):999-1005.

6. Bronzwaer SL, Cars O, Buchholz U, M├Člstad S, Goettsch W, Veldhuijzen IK, et al. A European study on the relationship between antimicrobial use and antimicrobial resistance. Emerg Infect Dis 2002;8(3):278-82.



7. Goossens H, Ferech M, Vander Stichele R, Elseviers M. ESAC Project Group. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005;365(9459):579-87.


8. Ministry of Health and Welfare. National Antibiotics Resistance Management Counterplan 2016Ōł╝2020 [Internet]. Sejong: Ministry of Health and Welfare; 2016. [Accessed August 11, 2016]. Available from:. http://www.motie.go.kr/common/download. do?fid=bbs&bbs_cd_n=81&bbs_seq_n=158481&file_seq_n=1..
9. Kim DS, Bae G, Lee HS, Kim HY, Kim SK, Um JS, et al. The study on evaluation of antibiotics use in outpatients with respiratory diseases. Wonju: Health Insurance Review & Assessment Service; 2010.
10. Tan T, Little P, Strokes T. Guideline Development Group. Antibiotic prescribing for self limiting respiratory tract infection in primary care: summary of NICE guidance. BMJ 2008;337:a437.


11. Kuyvenhoven MM, van Balen FA, Verheij TJ. Outpatient antibiotic prescriptions from 1992 to 2001 in the Netherlands. J Antimicrob Chemother 2003;52(4):675-8.


12. Seo OK. Inappropriate use of antimnicrobial agents in Korea and practical guidelines for its improvement. J Korean Soc Chemother 1997;15(2):201-3.
13. Cars O, M├Člstad S, Melander A. Variation in antibiotic use in the European Union. Lancet. 2001;357(9271):1851-3.


14. Brookes-Howell L, Hood K, Cooper L, Little P, Verheij T, Coenen S, et al. Understanding variation in primary medical care: a nine-country qualitative study of clinicians' accounts of the nonclinical factors that shape antibiotic prescribing decisions for lower respiratory tract infection. BMJ Open 2012;2(4):). pii: e000796..

15. Barden LS, Dowell SF, Schwartz B, Lackey C. Current attitudes regarding use of antimicrobial agents: results from physician's and paren's focus groups discussions. Clin Pediatr (Phila) 1998;37(11):665-71.



16. Trepka MJ, Belongia EA, Chyou PH, Davis JP, Schwartz B. The effect of a community intervention trial on parental knowledge and awareness of antibiotic resistance and appropriate antibiotic use in children. Pediatrics 2001;107(1):): E6..


17. Mangione-Smith. R, McGlynn EA, Elliott MN, McDonald L, Franz CE, Kravitz RL. Parental expectations for antibiotic, physician-parent communication, and satisfaction. Arch Pediatr Adolesc Med 2001;155(7):800-6.


18. Kim NS, Kim DS, Jeoung HJ, Kim CK, Kim MJ, Um JS, et al. Analysis and evaluation of antibiotics use. Wonju: Health Insurance Review & Assessment Service; 2006.
19. Kang MA, Son JY, Kim HJ. An exploratory application of the mixed methods research: application of surveys and focus group interviews for regional public health issue decision making. J Korean Public Admin 2007;41(4):415-37.
20. Morgan DL. Successful Focus Groups: Advancing the State of the Art. 1st ed.. Thousand Oaks (CA): SAGE Publications, Inc.; 1993.
21. Krueger RA, Casey MA. Focus Groups: A Practical Guide for Applied Research. 4th ed.. Thousand Oaks (CA): SAGE Publications, Inc.; 2009.
22. Lewis M. Focus group interviews in qualitative research: are-view of the literature [Internet]. NSW: The University of Sydney; 2000. [Accessed September 26, 2016]. Available from:. http://www.aral.com.au/arow/rlewis.html.
23. Coenen S, Van Royen P, Michiels B, Denekens J. Optimizing antibiotic prescribing for acute cough in general practice: a cluster-randomized controlled trial. J Antimicrob Chemother 2004;54:661-72.


24. Jang SN, Kim NS. Understanding the culture of antibiotics prescribing of primary physicians for acute upper respiratory infection. J Korean Acad Fam Med 2004;25(12):901-7.
-
METRICS

-
- 1 Crossref
- 0 Scopus
- 932 View
- 3 Download
- Related articles

 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


